*48 -year old female patient suffering from exertional dyspnea.



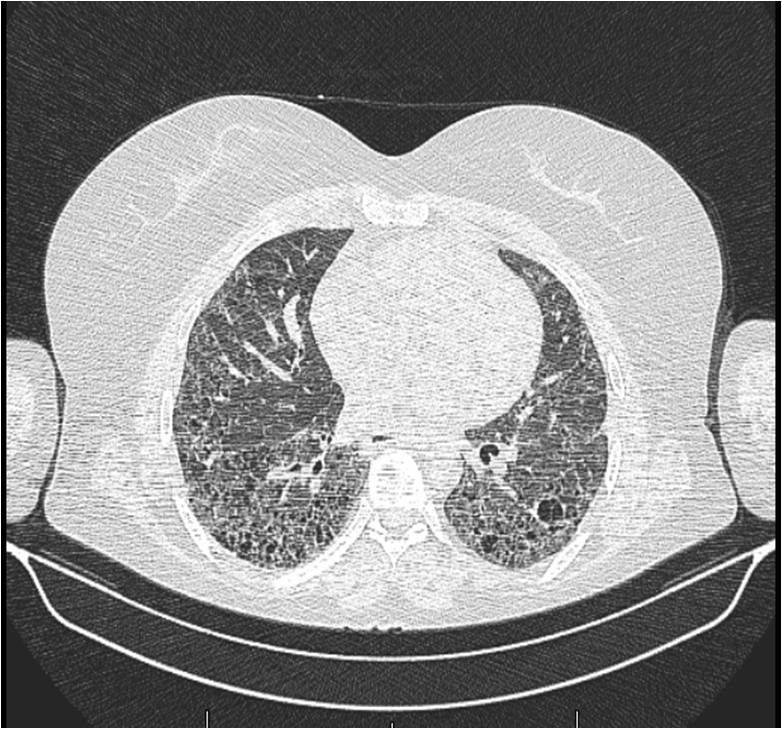
What is the most likely diagnosis?
1. Sarcoidosis
2. Silicosis
3. Scleroderma
4. Tuberculosis
Answer
Answer: Pulmonary involvement of scleroderma
Case Discussion:
Plain film demonstrates loss in lung volumes, coarse reticular interstitial pattern, and calcified mediastinal lymph nodes. HRCT revealed characteristic pulmonary fibrotic changes, typically in the lung bases and in the subpleural areas. These images show honeycomb change, intralobular septal thickening, dilated air-filled oesophagus, and pulmonary trunk widening (diameter larger than the adjacent ascending aorta). No pleural effusion is visible.
Only 25% of scleroderma patients present with respiratory symptoms or demonstrate abnormalities on CT. Pulmonary involvement of scleroderma is revealed histologically in 90% of patients with scleroderma. Although not pathognomonic, the combination of pulmonary fibrosis and a dilated esophagus is suggestive of scleroderma, especially in females (1).
Chest radiographs can appear normal in spite of respiratory function test abnormalities. Finally, changes of pulmonary fibrosis become apparent. Chest radiographs can show dilated oesophagus, calcification of mediastinal nodes, and enlargement of cardiac silhouette and pulmonary arteries due to pulmonary involvement of scleroderma Pleural effusions are rare (1). HRCT and CT scan can demonstrate features of interstitial lung disease. Early stages may show ground glass changes; later stages may illustrate honeycombing and evidence of lung volume loss, typically in the bases and in the subpleural lung, features of pulmonary hypertension. Pleural effusion is generally not a feature. A dilated esophagus is not an unusual finding (1, 2).
References:
1. Brant WE, Helms CA. Fundamentals of diagnostic radiology. Lippincott Williams & Wilkins. (2007).
2. Kim DS, Yoo B, Lee JS et-al. The major histopathologic pattern of pulmonary fibrosis in scleroderma is nonspecific interstitial pneumonia. Sarcoidosis Vasc Diffuse Lung Dis. 2002;19 (2): 121-7.
